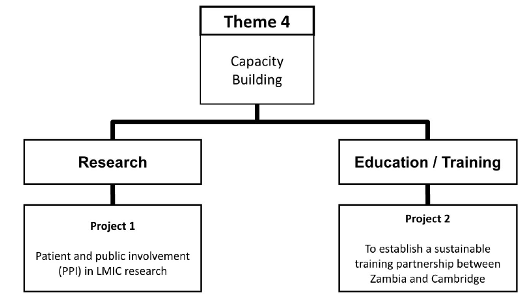
PROJECT 1 – How can we increase patient and public involvement in research?
Project Lead:
Background: While community engagement and involvement (CEI) is often embedded in most high income countries (HIC) research programmes, public involvement in research in LMICs is minimal and not well-documented (32). This is unfortunate as the benefits of public involvement in the design, conduct and dissemination of research have been shown to be significant in improving quality, and making studies more meaningful and relevant to the communities they serve (32). A notable tension that has been shown to exist when public involvement is attempted in LMIC studies is the dominant footprint of HIC models which are not generalisable to LMIC contexts where resources, environments and culture differ (32). In addition, the dominance of HIC led studies in LMICs can dilute the relevance of outcomes for local populations. Furthermore, there is also little evidence on the impact of public involvement or details of the strategy used (33). Given the importance of public involvement in research, it is necessary to address these gaps and issues in order for it to be ingrained in LMIC research.
Aims: To explore and evaluate models of community engagement and involvement that are most useful for acquired brain and spine injury research within LMIC settings. We propose a participatory action research methodology (PAR) which will enable us to utilise a problem-solving approach within a collaborative context working with LMICs researchers to embed CEI and explore barriers and facilitators to its implementation. To further ensure this we will provide mentoring, supervision, training and development opportunities for researchers and communities.
Target populations: This study will use a non-random, purposive approach to sampling which will recruit populations of researchers using CEI within identified projects and members of the local population who we engage in the CEI approaches used. As a qualitative study, the sample size will be small and informed by principles of data saturation. However, estimates for sample size are: n = 10 researchers and n = 20 members of the public.
Setting: Our intention is to start by embedding CEI into three studies within the Group’s portfolio (sites in Pakistan, Colombia and South Africa). However, we will discuss with collaborators to identify the most appropriate projects and networks to realise the ambition for CEI within the group.
Design framework: The aim of participatory action research methodology (PAR) is to understand and improve practice through action influenced by history, culture, and local context and embedded in social relationships (34). The participatory process should be empowering and lead to increased control for those involved. The PAR methodology will enable us to embed public involvement within three selected studies in this Group’s portfolio and explore how useful this was to their design and conduct.
Outcome measures: CEI will be evaluated through predominantly qualitative approaches, including semi-structured interviews and focus groups, to reach an in-depth understanding of the challenges and benefits of CEI and make recommendations for models of CEI that are most valuable with LMICs within the context of ABSI research.
Impact: By working in a participatory and collaborative way, we aim to facilitate CEI so that it becomes part of the research landscape within the participating sites beyond the life of this project.
PROJECT 2 - How can we develop a sustainable neurosurgery training programme in Zambia?
Project Lead:
Background: There is a severe shortage of neurosurgeons in LMICs. For example, in Africa, there are approximately 500 neurosurgeons for 1.2 billion people (35). Due to the severe shortage, it is estimated that 5 million individuals per year suffering from treatable neurosurgical conditions will never undergo a therapeutic surgical intervention (35). Sustainable development can only be met when infrastructure development is concomitant with human resources able to utilise and maintain resources. When the healthcare partnership between the Department of Neurosurgery at the University Teaching Hospital (UTH) in Lusaka and the NIHR Global Health Research Group on Neurotrauma began there were 2 fully trained neurosurgeons serving a population of 17 million in Zambia. A key development that was achieved as a result of the partnership was the development of Neurosurgery Training Curriculum and establishment of the first Zambian Neurosurgery Specialist Training Programme. The Programme is now in the third year and has recruited 7 residents, who are progressing through curriculum milestones. Aim: (1) To establish a sustainable training partnership between the Department of Neurosurgery at the University Teaching Hospital in Lusaka and the Department of Neurosurgery, Cambridge University Hospital in Cambridge based on a sustained exchange of trainees and fellows between the two countries. (2) To support training, we plan to establish a prospective, hospital-based registry of all cases with neurosurgical pathology admitted to University Teaching Hospital Lusaka.
Methods: We will establish a partnership with the International Surgical Training Programme (ISTP) of the Royal College of Surgeons of England (RCSeng) to develop a running 12-month Fellowship Programme in Neurosurgery for Zambian neurosurgery trainees. The Fellowship will recruit from trainees in their final years who have passed The College of Surgeons of East, Central and Southern Africa (COSECSA) membership exams (a recognised partner of the ISTP and RCSeng) to work at the Department of Neurosurgery, Cambridge University Hospital in Cambridge. The Fellows will be expected to participate in all clinical activities, including outpatient and inpatient management as well as surgical activities during their time in Cambridge. We will also explore the establishment of a Global Fellowship Programme open to final year neurosurgery trainees from UK and Europe to spend 12 months at the Department of Neurosurgery at the University Teaching Hospital in Lusaka aiming to facilitate ongoing research projects within the Department in Lusaka. Alongside the exchange programme, we will organise a yearly course in line with the Neurosurgery Training Curriculum for Zambia, which will be open to all trainees from the East and Central African Region. We will aim for the course to be conducted in a similar way to the European Association of Neurosurgical Societies Training Course over 4 cycles covering the breadth of neurosurgery. Building on the infrastructure developed by our collaboration during the Lusaka TBI Epidemiology (LUTE) study, we will establish a prospective, hospital-based registry of all neurosurgery patients presenting to UTH. In addition to collecting routine clinical data, detailed follow-up will be carried out by a neuropsychologist with experience with neurosurgical patients using previously developed functional, quality of life and neuropsychological outcome measures.
Impact: Developing neurosurgical services requires sustained partnerships and a working training programme. Increased neurosurgical capacity will lead to reduction in the burden of pathology, improved outcomes, as well as further exponential growth of the ancillary services, e.g. anaesthesia, intensive care, etc. With increased numbers of neurosurgeons, a more country wide service will be possible allowing patients from remote areas of Zambia to benefit.