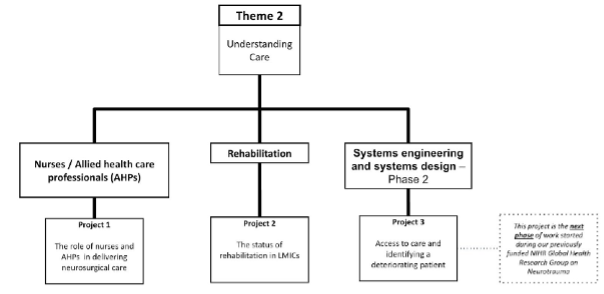
PROJECT 1 - What is the role of nurses and allied health professionals in providing effective neurosurgical care to ABSI patients?
Project Lead:
Background: Nurses and allied health care professionals (AHPs) are internationally recognised as a highly skilled workforce and essential to the delivery of safe effective patient care (15). Despite this, the nursing and AHP roles, and the contribution they make to patient care, is often understudied and/or undervalued. Nurses and AHPs in LMICs typically work with minimal budgets, limited resources and with patients who may be more often living in poverty and have complex health needs. In the context of neurotrauma there is a lack of adequately trained nurses and AHPs and this poses a challenge to the provision of adequate neurosurgical services (16). Therefore, as the largest component of the healthcare workforce, nurses and AHPs are strategically positioned to make a significant contribution to improving outcomes for patients following neurotrauma.
Aim: To examine the role of nurses and AHPs in delivering safe, effective and evidence-based neurosurgical care in LMICs.
Methods: Most LMIC research was led by high income countries (HIC) with little involvement of LMICs individuals or institutions. Cognisant of this bias in the evidence base this study will adopt a participatory methodology (17). Such methodology will facilitate a collaborative approach between HIC and LMIC researchers, increasing engagement, empowerment, and longer-term knowledge translation. To realise this ambition we will build on current relationships with colleagues in LMICs and create new ones. Nurse and AHP collaborators from India, the Philippines and Myanmar will be co-investigators and we will work together to develop appropriate methods to meet the aims of this study. This study will be qualitative and will adopt a constructivist epistemology that believes knowledge is constructed and commits to the presence of multiple realities.
Inclusion criteria: We will use a non-random, purposive approach to sampling. Principle inclusion criteria will be set with the aim of recruiting nurses and AHPs who are regularly providing care to neurotrauma patients in specific LMICs within the acute/sub-acute period.
Sample size: Sample size will be informed by principles of data saturation; however, we anticipate recruiting approximately 20-30 participants.
Data collection/Outcome measures: We anticipate using semi-structured interviews and focus-groups to collect data. We will provide training and development opportunities for collaborators in each country so that appropriate data collection can be undertaken in native languages. Online methods will be utilised if face to face data collection is still not possible due to the COVID-19 pandemic. Results will be analysed thematically.
PROJECT 2 - What is the status of rehabilitation services for ABSI in LMICs?
Project Lead:
Background: Rehabilitation post-TBI has been found to be an effective way of mitigating disability, particularly if it is delivered early and continues after discharge from hospital (18,19). While protocols and programmes for rehabilitation are common in most high-income countries (HICs), such services are lacking or unavailable in many LMICs (20). Given the importance of rehabilitation in the context of ABSI, it is necessary to explore this often-overlooked component of ABSI management.
Aims: (1) To document the current rehabilitation services/facilities available in Peshawar, Pakistan. (2) To carry out a needs assessment in order to understand what is required and what would make a difference. (3) To identify any barriers and facilitators to rehabilitation for TBI and how these can be addressed/overcome. (4) To develop and pilot a novel intervention that would aim to strengthen the delivery of rehabilitation locally.
Design framework: This mixed methods study, based on the Canadian Institutes of Health Research Knowledge- to- Action Framework (21), will begin with an audit on rehabilitation to assess availability. This entails reviewing the current evidence-base as well as studying documents and protocols pertaining to rehabilitation by way of document analysis. We will utilise qualitative methods by interviewing staff involved with neurorehabilitation to further understand what is being done from a practical perspective. Using a descriptive approach, we will seek to identify any gaps in the strategies and service provision as a whole and also speak to ABSI patients and/or their family members to understand the problems they face. These interactions (with patients and professionals) will not only give us an opportunity to ensure that the intervention we intend to implement will be not only beneficial and feasible in that context, but also inform the outcomes that would be measured subsequently. Candidate interventions include the development of educational videos for patients/carers, training of patients/carers on community-based therapy exercises etc. The next step would be a small-scale experimental study where the intervention will then be provided to a select number of patients who have received treatment for ABSI will be highly dependent on the local context, as well as the findings from the qualitative work. We will then measure the success of the intervention after a given period of time, both quantitatively and qualitatively.
Target population: For the qualitative work, we will use purposive sampling in order to recruit rehabilitation professionals who have experience working with ABSI patients. Similarly, we will recruit patients and/or carers. For the experimental study, the target population would be patients who need rehabilitation and/or carers (if participants are not able to provide qualitative input on the intervention). Setting: This project will be carried out in Pakistan. From previous work done in this setting, rehabilitation is an area of unmet need. Future plans are to extend this work to involve another LMIC, either India or Colombia.
PROJECT 3 - What service improvements can be made to increase access to care and identify a deteriorating patient?
Project Lead:
Background/Aims: The existing Group has focussed for the past three years on developing a systems understanding of neurotrauma care in Yangon, Myanmar, using qualitative research based around systems engineering and systems design theory. The second phase of this research work is to design specific interventions to address some of these needs, while also piloting new mixed-methods approaches to understanding healthcare through a systems-thinking lens. Access to care is the fundamental issue in terms of neurotrauma at Yangon General Hospital (YGH), and this can be considered at three stages: referral to the specialist centre, flow through the hospital once admitted, and recognition of deterioration once an inpatient. To examine these, we have devised three sub-projects:
Inpatient: The Yangon Early Warning Score (YEWS)
The pilot data for YEWS was collected during the first phase of the current Group under the project ASIA-TBI, and describes the experiences of family members caring for those with traumatic brain injury in YGH. This project will use this data to design a family-administered scoring system to allow earlier identification of deteriorating patients in situations where family members are the primary caregivers. We aim to design and pilot this scoring system and believe it will lay the groundwork for a future comparative effectiveness trial.
Admission: Data-driven modelling of patient flow within Yangon General Hospital and rearchitecting of care pathways within YGH for neurotrauma
This project involves a partnership formed between the GHRGN, the Departments of Engineering and Architecture at the University of Cambridge, and Article-25, an humanitarian architecture firm engaged by YGH to redesign their campus. The project aims to use the qualitative systems mapping from the first phase of the GHRGN work, along with data-driven approaches to understanding patient flow, to inform structural and procedural redesign of patient care at YGH. This involves understanding and improving where patients are managed, by whom, and with what resources.
Referral: Pathways within Myanmar for emergency paediatric neurosurgery
The aim of this project would be to create a programme that compliments the Emergency Treatment and Triage Plus course (ETAT+), developed by WHO, and the Myanmar Neonatal Care Programme, to look at improving the care of paediatric neurosurgical and trauma patients who present at district and community level facilities. This would involve a short training course and an ongoing programme to encourage quality improvement and local sustainable training. The course would focus on not only the immediate management and referral strategy, but also the transfer of sick children, which is a challenge in many lower income countries. A further goal would be to improve communication, and promote earlier referral, to tertiary specialists, including paediatric surgeons / neurosurgeons, to optimise care of these children.
Methods/Outcome measures
Inpatient: The Yangon Early Warning Score (YEWS). The research plan is to use the coded qualitative data to drive a tool design process in collaboration with Burmese colleagues. This will involve a Delphi process to determine which fields will be of most utility in a given tool, and then validation against established clinical scoring systems such as the Glasgow Coma Scale. Once this has been achieved, the tool will be piloted and subject to a comparative effectiveness trial.
Admission: Data-driven modelling of patient flow within Yangon General Hospital and rearchitecting of care pathways within YGH for neurotrauma. This will involve prospective data collection on TBI patient flow, including timestamps and locations. The feasibility of prospective data collection at YGH has been confirmed through participation in our previous GNOS-1 study. This data will be combined with GEO-TBI data to build quantitative network maps of YGH which will complement the qualitative maps built up over the preceding research programme. These will then be used to inform a re-architecture of both the hospital and the processes within it through collaboration with Article 25 (humanitarian architecture firm engaged by YGH to redesign their campus).
Referral: Pathways within Myanmar for emergency paediatric neurosurgery. This will involve course design, piloting and validation using established educational research methodologies.
The projects will continue to be integrated with the Cambridge Yangon Trauma Intervention Partnership and supported by Cambridge Global Health Partnerships, as well as working directly with THET Myanmar and the Rangoon General Hospital Reinvigoration Trust.